How Do Dentists Treat Sleep Apnea | Oral Appliance Therapy in Pennsylvania
Learn how dentists treat sleep apnea with oral appliance therapy, custom devices, and collaboration with sleep physicians. Find out if dental sleep medicine is right for you.
When most people hear “sleep apnea,” they immediately think of pulmonologists or sleep centers and CPAP machines. However, dentists — especially those trained in dental sleep medicine — play a critical role in diagnosing, treating, and managing many cases of obstructive sleep apnea (OSA).
In this article, we explore how dentists treat sleep apnea, what oral appliance therapy involves, how dentists collaborate with sleep physicians, and what patients can expect before, during, and after treatment.
1. The Dentist’s Role in Sleep Apnea Care
Dentists with specialized training in dental sleep medicine may help in various phases of sleep apnea care:
- Screening & risk evaluation: During routine dental exams, dentists can look for anatomical risk markers: large tongues, narrow airway space, retrognathia (receded jaw), high-arched palate, crowded or missing teeth, and reports of snoring or nocturnal breathing pauses. (Ada Association)
- Referral & diagnosis integrator: Dentists coordinate with a patient’s physician or sleep specialist to interpret sleep test results (home sleep test or in-lab polysomnography). (aadsm.org)
- Designing and fitting oral appliances: Once the diagnosis is confirmed and a prescription is issued, the dentist fabricates, fits, and adjusts a custom oral appliance that helps maintain airway patency during sleep. (aadsm.org)
- Follow-up, monitoring & adjustments: After delivery, dentists monitor patient comfort, compliance, side effects (jaw soreness, bite changes, tooth movement), and may order follow-up sleep tests to verify efficacy. (aadsm.org)
Dentists operating in dental sleep medicine often hold credentials recognized by the American Academy of Dental Sleep Medicine (AADSM) or board-level qualification (Diplomate of the American Board of Dental Sleep Medicine). (aadsm.org)
2. Oral Appliance Therapy: The Core Dental Treatment
The primary tool dentists use in sleep apnea treatment is oral appliance therapy (OAT) — especially for patients with mild-to-moderate OSA or those intolerant of CPAP. (Sleep Education)
How It Works
Oral appliances—often mandibular advancement devices (MADs)—hold the lower jaw forward (and sometimes stabilize the tongue) so that the upper airway remains open during sleep. (Sleep Education)
Some features and types:
- Custom vs non-custom: Custom, titratable appliances produced by a dentist outperform over-the-counter “boil-and-bite” devices in comfort, compliance, and effectiveness. (Ada Association)
- Single-piece vs dual-piece: 2 piece, adjustable appliances are recommended over boil and bite or Monoblock appliances as the Standard of Care.
- Titration: The dentist adjusts the appliance gradually (forward or back) to find the “therapeutic position” that balances airway opening with comfort. (aadsm.org)
Advantages of Oral Appliance Therapy
- Noninvasive & reversible: No surgery required, and the appliance can be discontinued if needed. (aadsm.org)
- Better compliance: Many patients find oral appliances easier to tolerate than CPAP masks, leading to higher nightly use. (aadsm.org)
- Comfort & portability: Small, quiet, and easy to travel with. (Sleep Education)
- Effectiveness: For many patients, OAT reduces the Apnea-Hypopnea Index (AHI), improves oxygen levels, lowers daytime sleepiness, and enhances quality of life. (Ada Association)
Limitations & Considerations
- Not As Overpowering As CPAP: With less side effects than pressurized CPAP devices, Less side effects then pressurized CPAP devices, and we have higher compliance then CPAP with less side effects.
- Side effects: Jaw discomfort, tooth or bite changes, temporomandibular joint (TMJ) symptoms, and irritation of soft tissues. These are usually manageable with adjustments and resolve with use of jaw exercises and a morning bite aligner. Less then 10% of patient discontinue use of an oral appliance due to side effects.. (aadsm.org)
- Need for regular monitoring: Long-term use may cause gradual tooth movement or bite shift, so periodic checks are essential. (aadsm.org)
Because of these trade-offs, patient selection and compliance are critical. Dentists must follow standards and guidelines (e.g. AADSM standards) to screen, treat, and monitor effectively. (aadsm.org)
3. The Dental-Sleep Physician Team: Collaboration Is Key
Sleep apnea is a medical condition, and dentists rarely work in isolation. For optimal patient outcomes, a multidisciplinary approach is standard:
- Prescription & oversight by a physician: A physician (typically a sleep specialist or pulmonologist) issues the diagnosis and prescription for treatment. The dentist’s appliance is part of that medical plan. (aadsm.org)
- Joint guidelines: The AASM and AADSM have published
joint clinical guidelines endorsing collaboration between dentists and physicians on oral appliance therapy. (AASM)
- Follow-up sleep testing: After appliance fitting and adjustments, physicians and dentists may order repeat sleep studies or home tests to confirm efficacy and adjust the therapy as needed. (aadsm.org)
- Comprehensive care plans: Many patients benefit from combining dental appliance therapy with weight loss, positional therapy, CPAP in hybrid form (if needed), or surgical options. (aadsm.org)
This team model ensures the patient’s airway, anatomy, medical risk, and device compliance all align.
4. What the Treatment Process Looks Like (Step by Step)
Here’s a generalized pathway a patient might follow at a clinic like Pennsylvania Dental Sleep Medicine (PDSM):
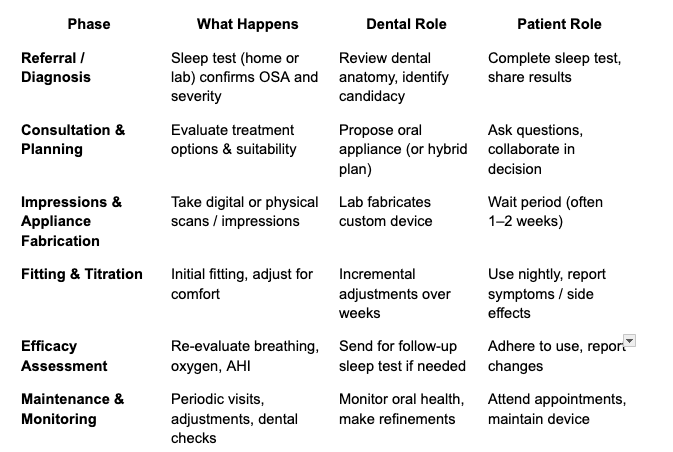
Many patients begin noticing improvements in daytime alertness, mood, energy within days to weeks — but optimal results typically require consistent nightly use and ongoing oversight.
5. Why Choose a Dentist-Trained in Sleep Medicine?
Not all dentists treat sleep apnea. Here’s what makes a qualified dental sleep provider stand out:
- Special training & credentials: A dentist with board-level dentistry/sleep credentials demonstrates greater expertise in airway science and appliance therapy.
- Following standards & evidence-based protocols: The AADSM’s “Standards for Screening, Treatment, & Management” offer updated protocols for care.
- Patient-specific, long-term focus: They can monitor bite changes, tooth health, side effects, and adjust therapy over years.
- Collaboration with physicians: A reputable dental sleep practice maintains active communication with sleep doctors to manage patient outcomes holistically.
- Comfort & compliance emphasis: A good provider ensures the appliance is tolerable, and is willing to adjust for comfort to boost long-term adherence.
At PDSM, Dr. Fox focuses on delivering comfortable, customized solutions — prioritizing patient compliance and long-term success.
Conclusion: Dentists Can Do More Than You Think
Dentists trained in dental sleep medicine are essential allies in the fight against sleep apnea. They screen, co-manage, fabricate, adjust, and monitor therapies like oral appliances — often providing a more tolerable alternative for patients who struggle with CPAP.
If you suspect sleep apnea or have been told you’d need CPAP, it’s worth discussing with a qualified sleep dentist like Dr. Fox in Harrisburg. Their tailored approach can lead to better comfort, better sleep, and better health outcomes — without sacrificing dental care or quality of life.
Next step: Schedule a consultation with Pennsylvania Dental Sleep Medicine to see if oral appliance therapy might be a good fit for you.


